In a breakthrough diabetes research, a team of scientists
from Harvard University, MIT, as well as from Boston Children's Hospital and
other centers has designed a biomaterial that can be used to encapsulate human
pancreatic cells before transplanting them.
Animal tests have shown that the implanted human pancreatic
cells can combat attack by the immune system in mice for up to 6 months, while
maintaining their ability to sense low blood sugar and produce insulin in
response.
Read more Type 2 Diabetes Cure? A Super Low-Calorie Diet May Be The Answer!
Read more Type 2 Diabetes Cure? A Super Low-Calorie Diet May Be The Answer!
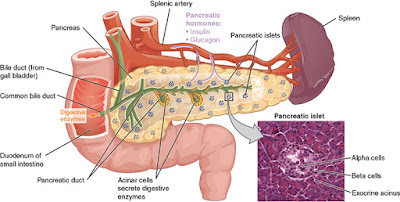
Type 1 diabetes happens when the islet cells located in oura
pancreas, are attacked by the immune system, and renders them unable to produce
insulin. Our body needs insulin – a type of hormone – to regulate glucose
(blood sugar).
Type 1 diabetes requires lifelong treatment to keep blood
sugar levels within a target range. Several times each day, patients with the
disease are required to check their glucose level, and to keep the level from getting
too high, they need to inject themselves with insulin.
Read more Type
2 diabetes linked to neurofibrillary tangles found in brain cells of
Alzheimer’s patients
One of the methods to improve type 1 diabetes treatments is by
replacing the damaged islet cells with healthy cells that is able to bring back
their ability to monitor glucose and release insulin. However, after trying in
numerous patients, the success of this method was found to be limited because
of the fact that the patients needed to take immunosuppressant medications for
the rest of their lives.
This newly discovered biomaterial is a by-product of alginate – a substance
originally derived from brown algae. Researchers discovered that cells can be
encapsulated with Alginate gels without injuring them and also permit molecules
like proteins and sugar to move through, enabling cells to sense and retort to
biological changes.
However, during the testing phase when gel capsules were implanted
in humans and primates, the researchers found that scar tissues eventually
covers the surfaces of the capsule, blocking molecules to pass through and
reducing the effectiveness of encapsulated devices.
The research team explained how they tested numerous different
types of alginate in the paper Nature
Biotechnology.
All the alginate derivatives were made by attaching various small
molecules to the chain of polymer, hoping that these modifications would make
them invisible to the immune system, explains Arturo Vegas of Boston
University.
They picked a strain of these rodents with a powerful immune system and then into their abdominal cavity, they implanted TMTD-encapsulated human islet cells.
Following implantation, in response to glucose, the cells immediately started making insulin and kept blood glucose under control for 174 days – the entire study period.
Read more Eating Tomatoes May Repair Lung Damage In Ex-Smokers
The exciting part was being able to display that in immune-competent mice, encapsulated cells do survive for an extended period, at least 6 months, said Omid Veiseh of the Boston Children’s Hospital.
The biomaterial was also tested as empty capsules, when the
researchers implanted it into the abdominal chambers of primates. These
capsules persisted for at least 6 months and did not accumulate scar tissue.
Researchers wanted to find out why this new biomaterial worked so
well. They found that the triazole ring present in it may impede the immune
system from recognizing the substance as foreign.
Senior research associate, Robert Langer, of Boston Children’s
Hospital said the combination of results from the two papers show that these
capsules can really shield transplanted cells in humans.
The next step for the team is to further test these materials in primates, aiming to eventually perform clinical trials in humans with diabetes.













No comments:
Post a Comment